A pressure ulcer is a localized injury to the skin or underlying tissues that occurs when there is a decrease in blood circulation caused by pressure applied to a specific area.
Initially, you may notice a slight redness in the affected area (the first sign of tissue damage). The underlying tissues undergo changes due to poor blood supply. Several layers of skin, muscles and bones can be affected.
All patients who are immobilized due to chronic illness or during the post-operative period are at high risk of developing pressure ulcers.
In the patient care program during their stay in hospital as well as at home, the patient and their family are informed about risk factors and preventive measures they should take to avoid the appearance of this type of ulcer.
If there is already a pressure ulcer, wound control is necessary, combined with the application of advanced dressings and the use of pressure-relieving devices.
Risk factors:
The main cause of tissue damage that leads to pressure ulcers is pressure build-up. Tissue damage is proportional to the intensity of the pressure and the duration of capillary compression.
Other factors that contribute to the risk of developing pressure ulcers:
- Aging
- Smoking
- Skin conditions: elasticity, edema, dryness
- Hypoxia in tissues, caused by underlying disease
- Nutritional abnormalities (overweight or underweight)
- Immunological abnormalities
- Neurological disorders
- Altered level of consciousness
- Incontinence
- Medication
- Reduced mobility, caused by pain, tiredness or stress
- Poor hygiene
- Unaware of the potential damage
Preventive measures:
Alternate the patient's position:
One of the simplest and most effective measures is to change the patient's position frequently.
- If the patient is unable to change position on their own, caregivers and healthcare providers should help them.
- Bedridden people should change position at least once every two hours.
- A person in a wheelchair should change position at least every 15 to 30 minutes.
If a pressure ulcer has already formed, it is important to prevent it from being subjected to additional pressure, either by repositioning it or by using pressure-relieving devices. This will give the wound a better chance of healing.
Follow a healthy and balanced diet:
A healthy, balanced diet with an adequate intake of proteins, vitamins and minerals helps prevent skin damage and will help wounds heal faster. If necessary, the patient can be referred to a nutritionist who will define a suitable diet plan for them.
Take care of your skin:
It's important to inspect the areas of the skin that are at risk on a daily basis. You can use a mirror to see the parts of the body that are more difficult to observe, such as the thighs and heels. If you notice any changes, discoloration of the skin (permanent redness, brownish color) you should contact your healthcare provider, family doctor or family nurse if you are at home, or one of your nursing assistants if you are in a hospital or nursing home.
Skin at risk:
Skin discoloration can indicate a grade 1 pressure ulcer, which must be properly treated before it causes further damage to the skin, which is often painful and usually takes a long time to heal.
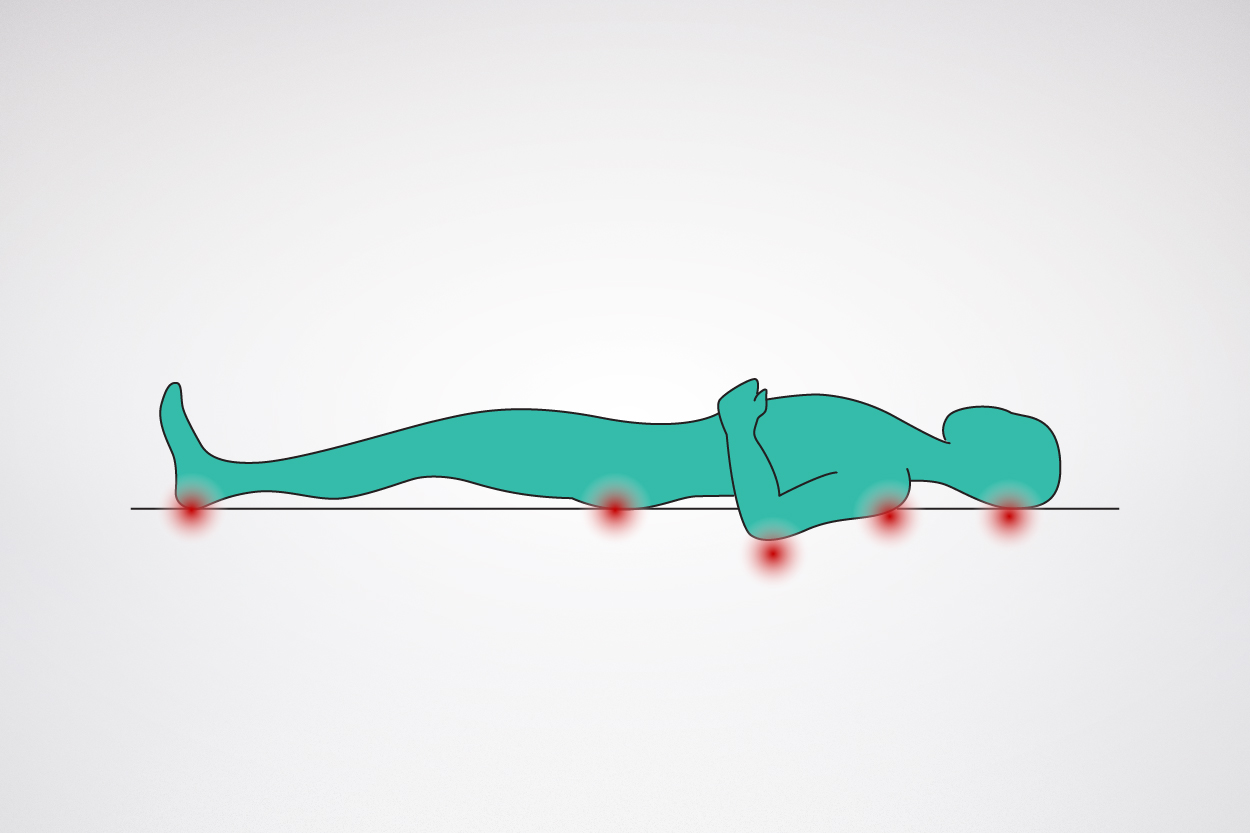
The elderly generally have dry and fragile skin. In conjunction with proper hygiene, topical application of products with essential fatty acids should be carried out, especially in areas at risk such as the heels, buttocks and elbows (see image for risk areas).
Prevention and skin care:
MoliCare® Skin Dermoprotective Cream with Zinc Oxide

Contains creatine, zinc oxide (20%), amino acids and almond oil. Works as a protective barrier in the genital area. With odor neutralizer.